11-11-2024
This is a synopsis of what has happened from start to finish, all in one post.
The events of this past week have been a vivid blur. There were many things that happened throughout this journey that were difficult to grasp and understand. Even now, only a few hours removed, I am sure that I am missing something. So, I would like to take a few moments to refresh us all on the things that have happened and make one more cohesive explanation of the situation from start to finish. Although some things will never truly be known, the conjecture presented here will be somewhat minimal. These are the events, understanding, and beliefs of myself and our family. (Without being too pointed, although there may be some stray opinion out there, please respectfully keep it to yourself. This is not the time, place, or situation in which to create division. To be clear, we have received a small amount of disagreement regarding a perceived “decision” that we made in which we “let our daughter go” or in other word killed Hannah. Confidence and boldness of opinion are often the luxury of ignorance.)
On Monday night, November 4, moments after I laid down to sleep. Janean burst in, saying that Hannah had eaten something with peanut in it. She had vomited already, broken out in a rash, was obviously uncomfortable, but in no way was she having any difficulty breathing. We left our house immediately and headed out to be with her. Only twice in her life had she actually encountered peanut to the point in which there was a reaction that took place. The first time was when she was three, she took a bite of a peanut butter cookie. As soon as she bit the cookie, before she could even think about chewing, she threw up and broke out in rash. This throwing up was immediate, then done, and the rash dissipated quickly, within a matter of a few minutes. So, it was at that point we knew that she had this allergy. We took her to the doctor, had her tested, and received our first “EpiPen”. At age six, basically the same thing happened. It was quick, thorough vomiting, with a rash that went away rather quickly. These were scarry events for sure, but in no way were they life threatening. Throughout the remaining years of her life, she would say, from time to time, that she could sense if something had peanut butter in it. Obviously, if the food was known to contain peanut, it was avoided. If for some reason, there was no way of knowing if there was peanut, if she touched it and even more so, if she brought it near her nose or mouth, she said that she would feel a strong negative reaction in her body. She would put the item back, and there was no reaction. Please remember that to some, just the smell of peanut, would trigger the reaction. This is so serious that the TSA banned open peanuts during air travel. Hannah’s allergy was not at that level.
As we drove to her side at Maranatha in Watertown, we kept her on the phone the entire time. She was obviously upset and uncomfortable but could breathe and speak clearly. We repeatedly told her to try to relax and reminded her that this type of reaction, though extremely unpleasant, was right in line with her previous experiences. We also repeatedly made it clear that she needed to try to calm down and focus on her breathing. If at any point she felt any tightness or difficulty breathing, she was to use the EpiPen immediately. While on the phone, we also texted a good friend who is a nurse and lives in Watertown. She quickly got to Hannah, evaluated the situation herself, and administered Benadryl. A few moments after this we arrived, and Janean ran up to Hannah and hung up the phone. Being a girl’s dorm, I waited outside. Janean found Hannah in the bathroom, shaken, but calming down and doing better. She suggested that with this improvement, perhaps Hannah should lie down on her bed. Hannah got up, walked to her bunk, climbed up the ladder, and laid down on her stomach all completely on her own without any need for assistance or concern. At this point over an hour had passed since she called us, the vomiting had subsided, and the rash was going away.
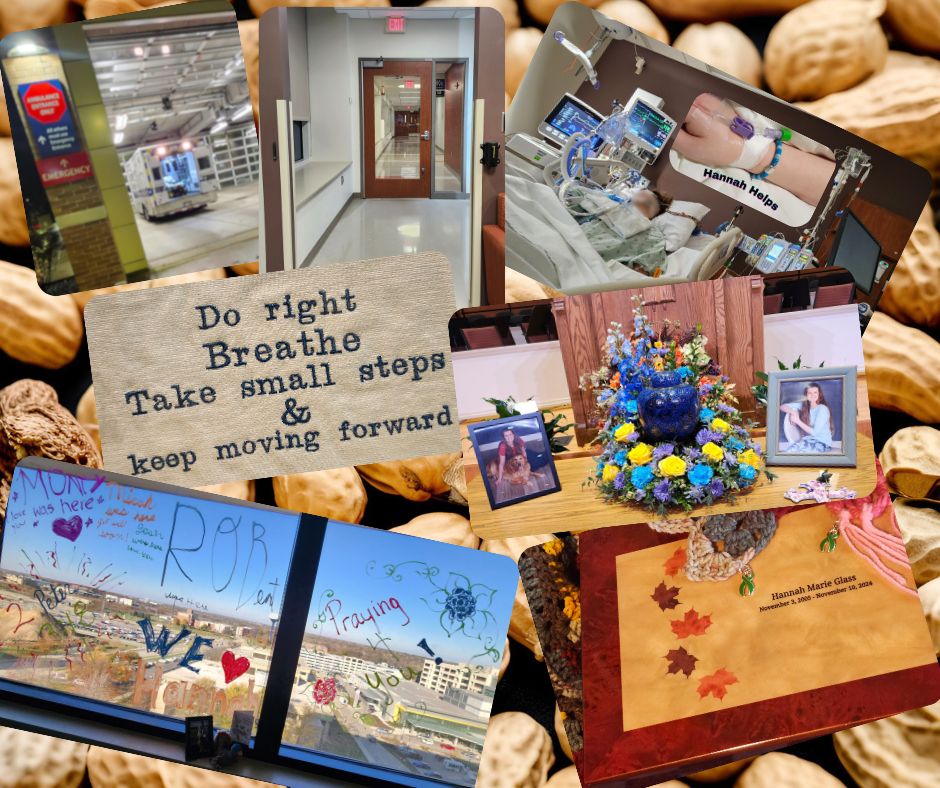
Janean told Hannah that perhaps laying on her stomach was not the best under these conditions, so Hannah rolled on to her side, then immediately curled up into the fetal position and began complaining of extreme shortness of breath and discomfort. She was told to get down and asked where her EpiPen was. She told the location of the pen, but while part way down the ladder she lost consciousness. The EpiPen was found and administered, and 911 was called immediately. Janean and those around her carried Hannah down the stairs to the entrance, where I met them. I picked her up facing me and carried her outside to wait for the ambulance to arrive. I had my foot on the running board of our vehicle, Hannah was on my knee facing me. My left hand held her up and my right held her head up. She was completely unresponsive, and I was incredibly helpless. The nurse monitored her pulse and remained on the phone with 911 dispatch until the EMTs arrived. Hannah had a weak thready pulse when I handed her over to them. They quickly moved her into the ambulance and began life saving measures. While in the ambulance, her heart stopped, but after 3-4 minutes they were able to restart it. A few minutes after she was in the ambulance, I left for the hospital so that I could meet them there. I abided by most traffic laws, made a phone call to each set of grandparents, missed my turn, drove past the hospital, turned around , found my way back, parked near what looked like an entrance, got out and ended up walking like halfway around the hospital trying to find out where to get in. Once inside, I spoke with the people at the desk, answered all questions, filled out the necessary paperwork, and then still had to wait until she arrived. Once Hannah was in the ER, I was escorted back to be with my wife in a waiting room. The doctor came in a couple of times saying that he placed her on a ventilator and the situation was not good. He was having difficulty being able to get her blood oxygen up. He also said that she would need immediate transfer to the first major hospital that could take her. Froedtert readily accepted her and wanted preliminary imaging and blood work to be done while transportation was arranged. Because of the weather, we were not able to get a med flight. Due to the fact that most ambulances are from local fire stations, it was difficult to get transport. (Local ambulances go from the station to the scene to the hospital, then return to the station, but we needed transport from hospital to hospital.) After transportation was arranged, it was more than an hour wait before they arrived. During that time, imaging revealed a collapsed lung on her right side. The doctor quickly inserted a chest tube and began suction. This greatly increased the blood oxygen level.
With her on the ventilator, the chest tube keeping her lung in position, and her heart beating on its own, we were able to be in the room, hold her hand, and talk to her for about ten minutes before the transport arrived. They came in, said that they needed a minute to adjust the chest tube for transport and that we should head to Froedtert so that we could get there near the same time as them. Janean and I returned to our car, stopped for gas, found our way to the correct hospital parking structure, called security for directions, signed in, and then waited perhaps another hour by security until they received word that Hannah had arrived. Without a patient, there could be no visitors let in for that patient, so we were stuck waiting.
Eventually we got upstairs to another waiting room where the first doctor told us that they had received the testing from Watertown hospital and also had begun their own testing. He told us that she had been without oxygen for a long time and that they were doing everything possible to help her. Also, he told us that she began having seizures between Watertown and Froedtert. This was an indication that her brain was severely damaged. Without getting into every detail of the next five days, it is easy enough to say that we were informed that the situation was bleak, but due to her age and good health, she was definitely going to be given every available opportunity and option to save her life. The ventilator kept her breathing, medication was administered to keep her heart going properly, and she was heavily sedated in order to prevent seizures or movement. X-rays, CTs, MRIs were all done alongside constant supervision and monitoring of the situation. We were not able to get more than one hour of uninterrupted sleep total in a night.
At around midnight Friday night, her heart rate began dropping. A CT was ordered and revealed that the damage to the brain was so significant that the deterioration of the dead tissues of the brain lead to an incredible amount of swelling. Due to the confinement of a skull, the brain was compressing the brains stem. This leads to the body shutting down completely. A neuro specialist was brought in and did a thorough evaluation of her condition. He then made a phone call. Then all the teams of doctors, each experts in their fields, met to discuss if there was any option left to save her. They spoke for forty-five minutes before arriving at the ultimate conclusion that even if they were able to reduce the swelling, the swelling was not the problem, but rather a symptom of the problem. The problem was that the majority of her brain was unmistakably, seriously, critically, and without the life sustaining measures in place, TERMINALLY damaged. There were no conversations regarding “quality of life” or anything like that. This was only life and death! At this point there was no actual decision to be made, except that we decided to donate her body to help others. So that they could have the chance at life that she no longer had, and to prevent other parents or loved ones from having to endure the torture that we had experienced over the previous week.
We met with Versiti, the organ donation group in our area. We were fully informed of the decision that we were making, including that unfortunate reality that in order to do this, we would have to wait another day and a half to allow the proper arrangements to be made: to line up recipients, their surgeons, and the travel necessary to coordinate the time sensitive donation process. To be clear, again, without the hard work of the medical professionals and the latest advancements in technology and medications, Hannah would have died, herself, Monday night. The only hard part of the decision to donate was having to wait. She was completely unaware, from the moment she lost consciousness, that anything was happening. There were never any true indicators of any improvement, but rather only signs that the damage was taking its toll. The adjustments in medication did lead to some basic brain stem reflexive responses at times, but by no means did “Hannah” ever remotely come back to us. The life sustaining measures taken, provided just enough opportunity for the minimal amount of less damaged brain tissue to operate in an extremely limited way.
While waiting for Versiti to make all necessary arrangements, and for the 2PM time on Sunday to arrive, Hannah deteriorated even further. Her blood pressure skyrocketed multiple times, and even more medications were needed to try to manage her condition. We had a meeting at this time in which we had to make the decision to resuscitate her in order to be able to save others. As hard as it was to realize that we had to let her go, it was now even harder to “hold her back”, for the sake of strangers, but it was the right thing to do and Hannah was “already gone”. We were only dealing with a body and the only ones suffering were us. So, after all the necessary arrangements were made, and we were one step away from the finish line, Hannah’s body was taken on an “Honor Walk” down to the operating room where we said our final goodbyes. Then she was wheeled into the OR where surgeons were ready to take what was necessary to save the lives of others.
Here is what we believe. When Hannah rolled on her side, the Anaphylaxis reaction that we had not seen before hit her incredibly hard. This caused her to gasp for breath, leading to the collapsing of the lung, further exacerbating the situation and making the ability of us, the EMTs, and the doctor at the Watertown hospital impossible to fix. Imaging cannot be performed under these conditions. The amount of time that lapsed until oxygen was restored was far too long to save her. At what time the soul, that unique God-given part of us, leaves the body is unknown. When the soul leaves, the body is dead. We believe that Hannah died the moment that she lost consciousness, or very shortly thereafter, and her loving heavenly Father took her immediately home to be with Him. We were left attempting to save a body these past days, but Hannah was already home Monday night. Monday night is when the brain died. God had a plan and God took her quickly. We suffered here, but she was and will forever remain free, and others have a chance to live!
We are blessed!
Many have asked if there’s any way in which to help us. Honestly, the two things that we need are your prayers and also, we could use help with the end-of-life expenses that are inevitable. It’s embarrassing to ask this, but at this point, this is the real physical help that we truly need. We were obviously not prepared for this. If there are, by some chance, more donations than we need, we have been in talks with Maranatha about setting up a scholarship in Hannah’s name, for students like Hannah to be able to get financial assistance. Thank you so much. Here is a link that you can click on to donate. If you would like to send a check, make it out to David Glass, and send it to Pederson-Nowatka Funeral Homes.
https://www.givesendgo.com/GDSPK
We are blessed!